Types of Acne | Acne Skin Guide
Acne vulgaris is a widespread chronic inflammatory skin condition affecting millions, occurring in various forms from mild comedones to severe cystic lesions. Non-inflammatory acne includes blackheads and whiteheads, while inflammatory lesions range from papules and pustules to deeper nodules and cystic acne. Multiple factors contribute to acne development, including hormones, genetics, diet, medications, and stress.
Treatment depends on severity, with over-the-counter topicals for mild cases and prescription medications or professional treatments for moderate to severe inflammatory acne. Severe cystic acne may require isotretinoin. Acne can lead to scarring, skin texture changes, and emotional impacts like low self-esteem. A comprehensive approach addressing the underlying causes, consistent skincare, and lifestyle changes is crucial for effective acne management under dermatological guidance to minimize potential complications.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Understanding the Different Types of Acne
Acne vulgaris, commonly referred to as acne, is one of the most prevalent skin conditions worldwide, affecting up to 50 million Americans annually. While often associated with adolescence, acne can occur at any age. This chronic inflammatory skin disease results from a complex interplay of factors, including hormones, excess oil production, bacteria, and inflammation. From mild comedones to severe cystic lesions, acne can manifest in various forms, each with its unique characteristics and treatment approaches.
Non-Inflammatory Acne: Blackheads and Whiteheads
Blackheads (open comedones) and whiteheads (closed comedones) are the mildest forms of acne and considered non-inflammatory lesions. Blackheads appear as small, dark spots on the skin’s surface, created when a hair follicle becomes clogged with excess oil and dead skin cells. The dark appearance is due to the oxidation of melanin, not dirt.
Whiteheads, on the other hand, are closed plugs within the follicle that appear as small, flesh-colored or white bumps on the skin’s surface. Both blackheads and whiteheads are often precursors to more inflammatory acne lesions and can be effectively treated with over-the-counter products containing salicylic acid or benzoyl peroxide.
Inflammatory Acne: Papules, Pustules, Nodules, and Cysts
When non-inflammatory acne lesions become infected with bacteria like Propionibacterium acnes, they can progress to inflammatory acne, characterized by redness, swelling, and potential scarring.
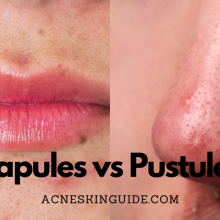
Papules are small, tender, red or pink bumps on the skin that signal the beginning of inflammatory acne. They occur when the hair follicle becomes inflamed but does not contain pus.
Pustules are similar to papules but are filled with pus, which gives them a yellow or whitish appearance. Both papules and pustules are considered mild to moderate forms of inflammatory acne and can often be treated with topical medications or oral antibiotics.
Nodules are large, solid, painful lesions that extend deeper into the skin. They are often firm to the touch and can last for weeks or months if left untreated.
Cystic acne, also known as nodulocystic acne, is the most severe form of inflammatory acne. These lesions are large, pus-filled cysts that extend deep into the skin and are often accompanied by inflammation and scarring. Cystic acne is challenging to treat and may require a combination of oral medications, such as isotretinoin (a vitamin A derivative), and professional treatments like corticosteroid injections or drainage procedures.
Downsides and Potential Complications
While acne is not a life-threatening condition, it can have significant physical and emotional impacts. Severe inflammatory acne, especially cystic lesions, can lead to permanent scarring, hyperpigmentation, and skin texture changes. These scars can be challenging to treat and may require professional treatments like chemical peels, microneedling, or laser resurfacing.
Moreover, acne can take a toll on an individual’s self-esteem and mental health, particularly during adolescence and young adulthood. The psychological impact of acne should not be underestimated, as it can lead to anxiety, depression, and social withdrawal.
Factors Contributing to Acne Development
Several factors contribute to the development and severity of acne, including:
- Hormones: Hormonal fluctuations, particularly during puberty, pregnancy, and menstrual cycles, can stimulate oil production and clogged pores, leading to acne breakouts.
- Genetics: Individuals with a family history of acne are more likely to develop the condition, as genetic factors can influence oil production, inflammation, and hormonal responses.
- Diet: While diet alone does not cause acne, certain foods high in refined carbohydrates and dairy products may exacerbate acne in some individuals.
- Medications: Certain medications, such as corticosteroids, lithium, and anabolic steroids, can contribute to acne formation.
- Stress: Increased stress levels can trigger hormonal changes and inflammation, potentially worsening acne.
Effective Treatment Strategies
The treatment approach for acne depends on the severity and type of lesions present. Mild to moderate acne can often be managed with over-the-counter topical treatments like benzoyl peroxide, salicylic acid, or retinoids. These products work by unclogging pores, reducing inflammation, and promoting cell turnover.
For moderate to severe inflammatory acne, prescription medications may be necessary. Oral antibiotics, such as doxycycline or minocycline, can help reduce inflammation and kill acne-causing bacteria. Hormonal treatments, like birth control pills or spironolactone, can be effective for hormonal acne in women.
In cases of severe cystic acne or persistent acne that does not respond to other treatments, isotretinoin (formerly known as Accutane) may be prescribed. This powerful oral medication effectively treats even the most stubborn cases but requires close monitoring due to potential side effects.
Professional treatments, such as chemical peels, laser therapy, or photodynamic therapy, can also be beneficial for more severe acne or scarring.
Maintaining a consistent skincare routine, avoiding harsh scrubbing or picking at lesions, and adopting a healthy lifestyle can also help manage and prevent acne breakouts.
Conclusion
Acne is a complex and multifaceted skin condition that can manifest in various forms, from mild blackheads to severe cystic lesions. Understanding the different types of acne and their underlying causes is crucial for effective treatment and management. While non-inflammatory acne can often be treated with over-the-counter products, inflammatory acne may require prescription medications or professional treatments. Additionally, addressing the emotional impact of acne and seeking support when needed is essential for overall well-being. By working closely with a dermatologist and adopting a comprehensive approach, individuals can successfully manage their acne and minimize potential scarring and complications.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Summary and FAQs
Are certain types of acne more common on specific areas of the body?
Yes, certain types of acne tend to be more common on specific areas of the body:
- Face: Blackheads, whiteheads, and inflammatory papules/pustules are most prevalent on the face, especially the forehead, nose, and chin areas.
- Back and shoulders: Inflammatory lesions like papules, pustules, nodules, and cystic acne are common on the back and shoulders. This type of body acne is often referred to as “bacne.”
- Chest: Similar to the back, the chest area is prone to inflammatory acne lesions, especially in those who wear tight-fitting clothing or sports gear that can cause friction and clogged pores.
- Neck: Blackheads, whiteheads, and inflammatory lesions can occur on the neck, especially the back of the neck or areas where hair products or cosmetics are applied.
- Scalp: Some individuals may experience acne on the scalp, which can manifest as pustules or cystic lesions around the hair follicles.
The distribution of acne lesions can vary from person to person and is influenced by factors such as hormones, genetics, and skin type. However, areas with a higher density of oil glands, such as the face, back, and chest, are generally more susceptible to different types of acne breakouts.
Can hormonal changes cause different types of acne?
Yes, hormonal changes can absolutely cause or influence different types of acne lesions. Hormones play a significant role in the development and severity of acne due to their impact on oil (sebum) production and skin cell behavior.
Here’s how hormonal changes can affect different types of acne:
- Blackheads and whiteheads (comedonal acne):
Fluctuations in hormones like androgens (male hormones) can stimulate increased sebum production, leading to clogged pores and the formation of blackheads and whiteheads. - Inflammatory acne (papules, pustules, nodules):
Hormonal changes can trigger inflammation in the skin, causing non-inflammatory comedones to progress into inflammatory lesions like papules (red bumps) and pustules (pus-filled bumps). Nodules (deep, painful lesions) can also develop due to hormonal influences. - Cystic acne:
Severe hormonal imbalances, especially during puberty, menstrual cycles, or hormonal treatments, can contribute to the development of cystic acne, which are large, pus-filled lesions deep within the skin.
Common hormonal events that can worsen or trigger different types of acne include:
- Puberty: Increased androgen levels during puberty often lead to comedonal and inflammatory acne.
- Menstrual cycles: Fluctuating estrogen and progesterone levels can cause premenstrual flare-ups of inflammatory or cystic acne.
- Pregnancy: Hormonal changes during pregnancy can trigger any type of acne, from blackheads to cystic lesions.
- Polycystic ovary syndrome (PCOS): This hormonal condition can cause increased androgen levels, contributing to acne breakouts.
Monitoring and managing hormonal imbalances is often a crucial part of treating and preventing different types of acne lesions, especially in women.
Is it possible to have multiple types of acne at the same time?
Yes, it is very common and possible to have multiple types of acne lesions present on the skin at the same time. Acne is a multi-faceted condition, and it is not unusual for an individual to experience a combination of different acne lesions simultaneously.
Here are some scenarios where someone might have multiple types of acne at once:
- Combination of non-inflammatory and inflammatory lesions:
Someone could have blackheads and whiteheads (non-inflammatory) along with papules and pustules (inflammatory) on different areas of their face or body. - Mixed severity levels:
An individual might have mild comedonal acne (blackheads/whiteheads) on some parts of their skin, while also experiencing more severe inflammatory nodules or cystic acne on other areas. - Different stages of acne development:
At any given time, there could be a mix of new lesions forming (microcomedones), existing non-inflammatory comedones, and inflammatory papules/pustules from previous breakouts. - Hormonal influences:
Hormonal fluctuations can cause various types of acne to flare up simultaneously, such as whiteheads, inflammatory papules, and even deep, cystic lesions.
The specific combination and distribution of acne lesions can vary greatly from person to person and may change over time due to factors like hormones, stress, medications, or treatment responses.
Having multiple types of acne at once is not uncommon and often requires a multi-pronged treatment approach targeting the different severities and types of lesions present.
Can certain types of acne be more difficult to treat than others?
Yes, certain types of acne can be more difficult to treat than others due to their severity, depth within the skin, and potential for scarring. Generally, the more inflammatory and severe the acne lesions, the more challenging they are to treat effectively.
Here’s a look at how the treatability of acne can vary based on the type of lesions:
- Blackheads and whiteheads (non-inflammatory comedones):
These are usually the easiest types of acne to treat as they are superficial and can often be managed with over-the-counter topical treatments containing ingredients like salicylic acid, benzoyl peroxide, or retinoids. - Papules and pustules (inflammatory lesions):
These inflammatory acne lesions can be more stubborn to treat than comedones, especially if they are widespread or recurring. Topical treatments may not be enough, and prescription oral medications like antibiotics or spironolactone may be required. - Nodules and cystic lesions:
These are among the most difficult types of acne to treat effectively. Nodules extend deep into the skin, and cystic lesions are large, inflamed, pus-filled bumps that can cause significant scarring if not treated properly. Oral isotretinoin (Accutane) is often prescribed for severe cystic acne that does not respond to other treatments.
In addition to the type of lesion, other factors that can make acne more challenging to treat include:
- Hormonal imbalances: Hormonal acne, especially during puberty or menstrual cycles, can be resistant to treatment until the underlying hormonal triggers are addressed.
- Duration of acne: Long-standing, persistent acne that has been present for years may be more difficult to resolve than recent-onset acne.
- Scarring: Acne that has already led to significant scarring may require additional treatments like chemical peels, laser therapies, or surgical procedures.
The best approach is to seek guidance from a dermatologist, who can assess the type and severity of acne present and develop an appropriate, potentially combination treatment plan tailored to the individual’s needs.