Papules vs Pustules | Acne Skin Guide
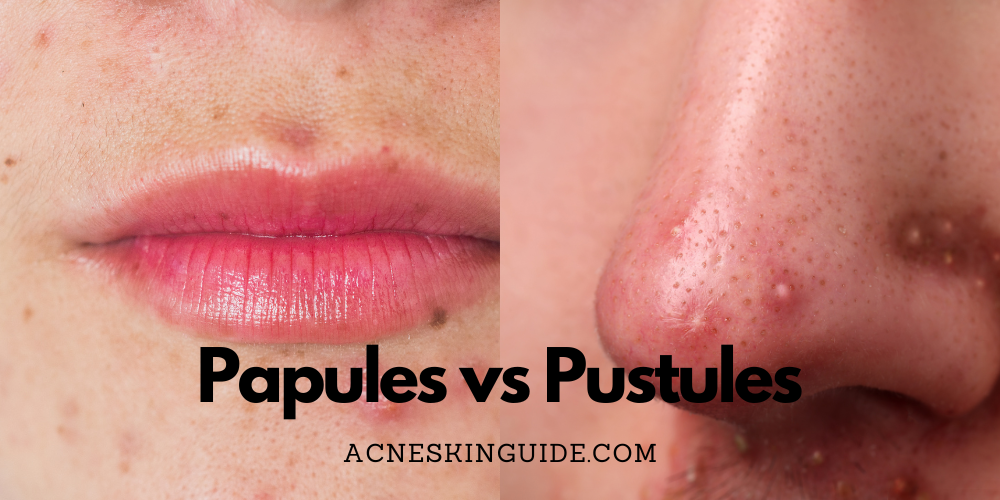
Distinguishing between acne papules and pustules is crucial for effective treatment. Papules are small, solid, red bumps caused by clogged hair follicles, while pustules are inflamed pus-filled lesions that typically develop from papules when further infected. Key differences include inflammation level, appearance, pain, healing time, and scarring risk – pustules being more inflamed, pus-filled, painful, longer to heal, and more likely to scar.
Proper identification through self-examination or consulting a dermatologist guides appropriate treatment, like over-the-counter products for papules versus prescription medications for pustules. Potential downsides include skin irritation, antibiotic resistance, scarring from improper care, and variability in individual responses. While home remedies may help mildly, seeking professional dermatological care is recommended for severe or persistent acne to minimize progression and scarring.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Understanding Acne Papules vs Pustules: A Comprehensive Guide
Acne is one of the most common skin conditions affecting millions worldwide. While often associated with adolescence, it can persist into adulthood. Acne lesions come in various forms, with papules and pustules being two of the most prevalent. Distinguishing between these two types is crucial for effective treatment and preventing further acne progression or scarring.
What are Acne Papules?
Papules are small, solid, rounded bumps that form on the skin, typically less than 1 cm in diameter. They develop when hair follicles become clogged with excess oil (sebum), dead skin cells, and bacteria, leading to localized inflammation. Papules appear as raised, reddish or pink bumps with no visible fluid or pus.
The formation of papules is often linked to hormonal fluctuations, particularly during puberty, menstrual cycles, or certain medical conditions. Genetics also play a role, as some individuals may be predisposed to excessive oil production or abnormal shedding of skin cells within the follicles. Certain skincare products, harsh scrubbing, or irritating substances can also contribute to the development of papules.
What are Acne Pustules?
Pustules, on the other hand, are inflamed, pus-filled lesions that typically develop from papules. When a papule becomes further irritated or infected, white blood cells rush to the area, accumulating and creating a white or yellow-headed blemish filled with fluid or pus.
The presence of pus in pustules is a result of the body’s immune response to bacteria, such as Propionibacterium acnes, which commonly reside on the skin and can proliferate within clogged follicles. Excessive squeezing, picking, or trauma to existing papules can also introduce bacteria and contribute to the formation of pustules.
Key Differences Between Papules and Pustules
While both papules and pustules are inflammatory acne lesions, there are several key differences:
- Inflammation Level: Pustules are more inflamed and swollen than papules, with visible pus indicating a heightened immune response.
- Appearance: Papules appear as solid, red/pink bumps, while pustules have a distinct white or yellow pus-filled center.
- Pain and Discomfort: Pustules are generally more painful and tender to the touch due to the increased inflammation and pus accumulation.
- Healing Time: Pustules tend to take longer to heal compared to papules, as the body needs to clear the infection and reduce inflammation.
- Scarring Risk: While papules rarely lead to scarring, if not properly treated, pustules have a higher risk of causing acne scarring, especially if picked at or squeezed.
Identifying Papules vs. Pustules
Proper identification of papules and pustules is essential for effective treatment. Here are some tips:
- Self-Examination: Carefully examine your skin in good lighting, using a magnifying mirror if needed. Look for the distinctive characteristics of each lesion type.
- Seek Professional Assessment: If you have severe, persistent, or widespread acne lesions, consult a dermatologist for an expert evaluation and diagnosis.
Treatment Considerations
The treatment approach for papules and pustules may differ due to their distinct characteristics:
- Treating Papules: Over-the-counter (OTC) topical treatments containing salicylic acid, benzoyl peroxide, or retinoids can help unclog pores and reduce inflammation in papules. Gentle exfoliation may also be beneficial.
- Treating Pustules: More aggressive treatment is often required for pustules. Prescription-strength topical medications like antibiotics or stronger retinoids may be prescribed. In some cases, oral antibiotics or isotretinoin (for severe cases) may be necessary to control inflammation and bacteria.
- Lifestyle Factors: Diet, stress management, and hormonal balance can also impact acne severity. Addressing these factors through a balanced diet, stress-reduction techniques, and hormonal treatment (if applicable) can support overall acne management.
Potential Downsides and Considerations
While effectively treating acne lesions is crucial, there are a few potential downsides and considerations to keep in mind:
- Skin Irritation: Some topical acne treatments, especially those containing benzoyl peroxide or retinoids, can cause dryness, redness, or irritation, especially when first starting treatment. Introducing new products gradually and using moisturizers can help minimize these side effects.
- Antibiotic Resistance: Overuse or prolonged use of topical or oral antibiotics for acne treatment can contribute to antibiotic resistance. It’s essential to follow a dermatologist’s guidance and consider alternative treatments when appropriate.
- Scarring Risk: While papules rarely scar, picking, squeezing, or improperly treating pustules can increase the risk of acne scarring. It’s crucial to avoid picking or popping pustules and seek professional guidance for proper treatment.
- Time and Persistence: Acne treatment can be a long-term process, and it may take several weeks or months to see significant improvement. Patience and consistent adherence to the prescribed treatment regimen are crucial for optimal results.
- Individual Variability: Every individual’s skin is unique, and what works for one person may not work for another. Personalized treatment plans tailored to one’s skin type, severity, and individual factors are essential for effective acne management.
Home Remedies and Professional Care
While some home remedies like tea tree oil, green tea, or honey may provide mild relief for mild acne, it’s crucial to seek professional care from a dermatologist for persistent, severe, or widespread acne cases. A dermatologist can properly evaluate the condition, recommend appropriate treatments, and provide guidance on managing acne effectively and minimizing the risk of scarring.
In conclusion, understanding the differences between acne papules and pustules is essential for optimal treatment and prevention of acne progression. Proper identification, targeted treatment approaches, and addressing underlying factors can help manage acne effectively while minimizing potential downsides like scarring or skin irritation. Remember, seeking professional guidance from a dermatologist is recommended for severe or persistent acne cases.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Summary and FAQs
Can papules turn into pustules, or are they separate types of acne lesions?
Yes, papules can turn into pustules. They are not entirely separate types of acne lesions, but rather represent different stages in the progression of inflammatory acne.
Papules are the initial solid, red bumps that form when a hair follicle becomes clogged and inflamed. If the inflammation and blockage persist, the papule can progress into a pustule.
As the follicle remains blocked, more white blood cells rush to the area to fight off bacteria and infection. This buildup of white blood cells, pus, and other fluids causes the previously solid papule to develop a visible white/yellow pus-filled center, becoming a pustule.
So in many cases, pustules evolve from pre-existing papules that have become more inflamed and infected over time. However, it’s also possible for some pustules to form directly without starting as papules first.
The key is that papules represent an earlier, less severe stage of inflammatory acne compared to the more inflamed, pus-filled pustular stage. Proper treatment of papules can help prevent them from progressing into more problematic pustules.
How long do papules and pustules typically last, and what factors influence their duration?
The duration of papules and pustules can vary, and several factors influence how long they last:
Papules:
- Typically last 3-7 days if properly treated
- May last 1-2 weeks or longer if untreated
- Factors like skin type, hormone levels, and treatment regimen affect duration
Pustules:
- Usually last 5-10 days
- Can persist for weeks if not treated properly
- More inflamed/severe pustules tend to have a longer healing period
Factors influencing duration:
- Treatment – Papules and pustules resolve faster with appropriate treatment using medicated creams, oral antibiotics, etc. Untreated lesions last longer.
- Skin Type – Those with oilier skin may experience longer lasting papules/pustules.
- Picking/Popping – This can prolong healing and lead to more inflammation.
- Hormone Levels – Fluctuations can cause persistent acne flare-ups.
- Hydration – Proper hydration supports faster healing.
- Stress Levels – Higher stress can worsen and prolong inflammatory acne.
- Skincare Routine – Using correct, non-irritating products aids faster resolution.
- Medications – Certain medications like birth control can help shorten acne duration.
In general, pustules being more inflamed lesions, tend to have a longer healing period compared to papules if not treated promptly and effectively. Following proper treatment and skincare is key to minimize duration.
Are there any specific triggers or activities that can increase the risk of developing papules or pustules?
Yes, there are several specific triggers and activities that can increase the risk of developing papules or pustules:
- Hormonal changes: Fluctuations in hormones, such as during puberty, menstrual cycles, pregnancy, or conditions like polycystic ovary syndrome (PCOS), can stimulate excess oil production and clogged pores, leading to papules and pustules.
- Friction or pressure: Activities that involve friction or pressure on the skin, such as wearing tight clothing, carrying heavy backpacks, or resting the face on hands, can worsen acne by irritating existing lesions or causing blockages in hair follicles.
- Sweating: Intense physical activity or exposure to heat and humidity can cause excessive sweating, which can mix with oils and bacteria on the skin, clogging pores and potentially triggering new papules or pustules.
- Certain medications: Some medications, such as corticosteroids, anabolic steroids, and certain psychiatric medications, can increase the risk of acne by affecting hormone levels or causing other side effects that contribute to clogged pores.
- Stress: High levels of stress can trigger hormone imbalances and inflammation, both of which can exacerbate acne and lead to the formation of papules and pustules.
- Cosmetic products: Heavy or comedogenic (pore-clogging) cosmetic products, such as oils, creams, and makeup, can block pores and contribute to the development of acne lesions.
- Environmental factors: Exposure to pollution, high humidity, and certain occupational settings (e.g., working with oils or greases) can increase the risk of clogged pores and subsequent acne lesions.
It’s important to note that while these triggers can increase the risk, individual susceptibility and underlying factors also play a role. Identifying and minimizing exposure to specific triggers, combined with proper skincare and treatment, can help manage and prevent the development of papules and pustules.
Can certain types of makeup or skincare products worsen or prevent the development of papules and pustules?
Yes, certain types of makeup and skincare products can definitely influence the development and severity of papules and pustules.
Products that can worsen papules and pustules:
- Comedogenic cosmetics: These products contain pore-clogging ingredients like heavy oils, petrolatum, or certain waxes. They can contribute to the formation of new papules and pustules by blocking pores.
- Heavy, occlusive makeup: Thick, oil-based foundations, concealers, and creams can trap oils, dirt, and bacteria on the skin, leading to clogged pores and new acne lesions.
- Skincare products with irritating ingredients: Products containing harsh surfactants, alcohol, fragrance, or other irritants can cause inflammation and disrupt the skin’s barrier, potentially exacerbating existing papules or triggering new ones.
Products that can help prevent papules and pustules:
- Non-comedogenic cosmetics: Look for oil-free, non-comedogenic (non-pore-clogging) makeup labeled as such. These are less likely to contribute to clogged pores.
- Salicylic acid and benzoyl peroxide products: These acne-fighting ingredients help unclog pores and reduce inflammation, preventing new papules and pustules from forming.
- Gentle, fragrance-free skincare: Using gentle, non-irritating cleansers, moisturizers, and serums can help maintain a healthy skin barrier and avoid inflammation that triggers acne lesions.
- Mineral-based makeup: Mineral-based foundations and powders tend to be less pore-clogging and can allow the skin to breathe better, reducing the risk of new acne lesions.
It’s also essential to remove all makeup and cleanse the skin thoroughly before bedtime to prevent clogged pores overnight. Additionally, regularly cleaning makeup brushes and tools can help prevent the transfer of acne-causing bacteria.
The key is to choose makeup and skincare products formulated for acne-prone skin and to follow a consistent, gentle routine to keep pores clear and minimize inflammation.
Are there any dietary or supplement recommendations specifically for managing or preventing papules and pustules?
While there is no definitive “acne diet”, certain dietary and supplement adjustments may help manage and prevent papules and pustules for some individuals:
- Increase intake of anti-inflammatory foods: Foods rich in omega-3 fatty acids (like salmon, walnuts, flaxseeds), antioxidants (berries, green tea), and zinc (pumpkin seeds, cashews) may help reduce inflammation that contributes to acne.
- Limit high-glycemic foods: Refined carbs, sugary foods/drinks can spike insulin and hormones like IGF-1, potentially worsening acne. Opt for low-glycemic alternatives.
- Probiotic and prebiotic foods: Fermented foods with live probiotics (yogurt, kefir, kimchi) and prebiotic fibers may promote a healthier gut microbiome linked to clearer skin.
- Omega-3 supplements: Fish oil or algae oil supplements providing EPA and DHA can have anti-inflammatory effects potentially beneficial for acne.
- Zinc supplements: Zinc plays a role in wound healing and has anti-inflammatory properties. Moderate zinc supplementation may reduce acne severity for deficient individuals.
- Spearmint tea/supplements: Compounds in spearmint may help reduce male hormone levels linked to acne.
- Avoid dairy: Some studies link milk (due to hormones/sugars) to increased acne severity. Try limiting dairy to see if it helps.
- Stay hydrated: Proper hydration supports overall skin health and may help manage acne.
Dietary changes alone won’t “cure” acne, but can provide adjunctive benefits when combined with medical acne treatments. Individual responses vary, so tracking one’s diet and consulting a dermatologist is recommended before significantly altering nutrient intake.