Acne Vulgaris Symptoms | Acne Skin Guide
Acne vulgaris is a chronic inflammatory skin disorder distinct from occasional acne breakouts. It results from excess oil production, clogged pores, bacterial overgrowth, and inflammation, often triggered by hormonal changes. Inflammatory lesions like papules, pustules, nodules, and cysts characterize acne vulgaris, along with non-inflammatory blackheads and whiteheads. Unlike typical pimples, acne vulgaris is more widespread, cyclical, and can lead to scarring.
Beyond physical effects, it significantly impacts self-esteem and mental health. While often confused with conditions like rosacea or folliculitis, proper diagnosis by a dermatologist is crucial. Treatment involves over-the-counter or prescription topicals, oral medications, and may require combination therapy for severe cases. Although management can be challenging with potential side effects, understanding acne vulgaris’ distinct nature guides appropriate treatment for symptom relief over time with realistic expectations for this chronic condition.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Acne Vulgaris: Understanding This Chronic Inflammatory Skin Condition
When it comes to acne, there’s more than meets the eye. While many people use the term “acne” to describe the occasional pimple or breakout, there is a specific condition known as acne vulgaris that presents unique challenges. This chronic inflammatory skin disorder is characterized by recurring bouts of inflammatory lesions like pimples, cysts, and nodules. Let’s dive deeper into what acne vulgaris is and how it differs from typical acne flare-ups.
The Underlying Causes
Acne vulgaris results from a complex interplay of factors including excess oil production, clogged pores, bacterial overgrowth, and inflammation. The key culprit is often hormonal changes that stimulate increased sebum (oil) production. This excess oil can mix with dead skin cells and bacteria, clogging pores and hair follicles. The clogged follicles provide an ideal environment for bacteria like Propionibacterium acnes to multiply rapidly, leading to inflammation.
Types and Presentation
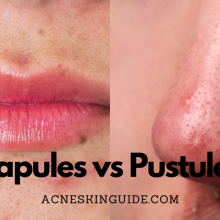
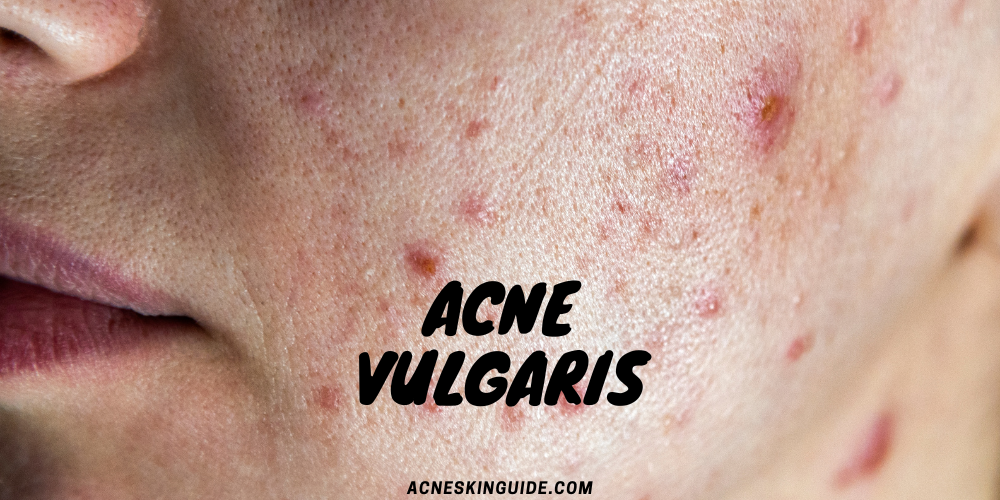
There are two primary types of acne vulgaris lesions – inflammatory and non-inflammatory. Inflammatory lesions include painful papules, pustules (pimples), nodules, and cysts. Non-inflammatory lesions refer to the more common blackheads and whiteheads. In mild cases, blackheads, whiteheads, and small pimples may be present. However, severe acne vulgaris can manifest as large, painful nodules and cysts that increase the risk of permanent scarring.
Unlike the occasional pimple, acne vulgaris tends to be more widespread, affecting areas beyond just the face like the back, chest, and shoulders. It also cycles through periods of remission and flare-ups rather than being consistently present or quickly resolving.
Impacts on Physical and Mental Health
The effects of acne vulgaris extend beyond just physical symptoms. Active lesions can lead to scarring, skin discoloration, and damage to the surrounding skin. However, the psychological impacts are just as significant. Dealing with persistent inflammatory breakouts can take a major toll on self-esteem and quality of life, especially during adolescence. Complications like anxiety, depression, and social withdrawal are common among those with severe acne vulgaris.
Differentiating Similar Conditions
While often used interchangeably, acne vulgaris is distinct from other acne-like skin conditions. Acne rosacea causes redness, flushing, and small bumps primarily concentrated on the face. Folliculitis refers to inflammation of the hair follicles leading to small pimple-like bumps. Another condition sometimes mistaken for acne is pityrosporum folliculitis, which results from an overgrowth of yeast rather than bacteria. Proper diagnosis by a dermatologist is crucial to determine the appropriate treatment approach.
Treatment Landscape
Over-the-counter topical treatments for mild acne vulgaris include benzoyl peroxide, salicylic acid, and retinoids like adapalene. For moderate to severe cases, prescription oral and topical medications are typically required. Some common prescription options include oral antibiotics to reduce bacterial levels, isotretinoin (a potent vitamin A derivative), hormonal therapies, and topical retinoids.
In recent years, there has been increasing interest in natural and alternative remedies for acne vulgaris aimed at reducing inflammation and bacterial overgrowth. Options like tea tree oil, green tea, probiotics, and dietary changes show some promise but require more research.
No matter the treatment approach, it’s important to have realistic expectations. Most acne vulgaris treatments take 2-3 months to see full results. Combination therapy using medications from different classes is often necessary for severe, treatment-resistant cases to achieve adequate clearing.
It’s also important to weigh potential side effects, which may include dryness, irritation, sun sensitivity, headaches, and gastrointestinal issues depending on the specific medication.
Prevention and Risk Factors
While there is no surefire way to prevent acne vulgaris, there are steps that may help reduce flare-ups in some individuals. Following a consistent skincare routine, managing stress levels, hormonal treatments, and avoiding certain medications that can exacerbate acne may provide benefits. However, acne vulgaris often has a strong genetic component, so managing expectations is key.
The Downsides
Despite the variety of treatment options available, acne vulgaris remains a challenging and often chronic condition for many people. Clearing can take months and full remission is difficult to achieve, with stubborn lesions and scarring persisting in some cases. The physical and emotional impacts, potential side effects of medications, and the relapsing nature of acne vulgaris can take a significant toll. It requires ongoing management, which can become frustrating and impact quality of life.
Closing Thoughts
Acne vulgaris is more than just an inconvenient breakout. This inflammatory skin condition has distinct causes, presentations, and treatment needs compared to typical acne. By understanding these differences, individuals can work closely with a dermatologist to receive an accurate diagnosis and explore the most appropriate therapies. With proper care and management, many can find relief for their acne vulgaris symptoms over time. However, it’s important to have realistic expectations, as this chronic condition often requires ongoing vigilance.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Summary and FAQs
Is acne vulgaris contagious or can it be spread from person to person?
No, acne vulgaris is not contagious and cannot be spread from person to person. It is caused by a combination of factors like excess oil production, clogged pores, bacterial overgrowth, and inflammation – not by transmission between individuals.
While the acne-causing bacteria Propionibacterium acnes can potentially be spread through direct skin contact or sharing personal items like towels or pillowcases, simply being exposed to this bacteria does not cause acne vulgaris in someone who is not already predisposed to developing it.
Acne vulgaris develops due to an individual’s own factors like hormones, genetics, and abnormal skin cell shedding within the hair follicles. The bacteria alone is not sufficient to cause acne vulgaris in someone whose follicles are not already clogged and primed for acne formation.
So in summary, you cannot catch acne vulgaris from someone else who has it. The condition is not transmissible between people. Proper hygiene can help reduce acne-causing bacteria on the skin, but acne vulgaris itself does not spread through any kind of contagious process.
Are there different types of acne vulgaris based on severity?
Yes, acne vulgaris is often categorized into different types or grades based on its severity. The classification is typically done by evaluating factors like the types of acne lesions present, the extent and distribution of breakouts, and the risk of developing permanent scarring.
Some common ways acne vulgaris is graded by severity include:
Mild Acne Vulgaris
- Primarily consists of non-inflammatory lesions like blackheads and whiteheads
- May have some small inflammatory papules and pustules
- Usually confined to a limited area like the face
Moderate Acne Vulgaris
- Mix of inflammatory lesions (papules, pustules) and non-inflammatory comedones
- Lesions more widespread, can affect the face, back and chest areas
- May lead to minor scarring if lesions are picked/popped
Severe Acne Vulgaris
- Predominance of inflammatory lesions like nodules and cysts
- Widespread on the face, back, chest and shoulders
- Lesions are often large, painful and have high risk of causing permanent scarring
- May also have many comedones present
In severe cases, acne vulgaris may also be classified as severe nodular acne or severe cystic acne when the inflammatory lesions are particularly large, widespread and likely to cause scarring.
Grading the severity helps guide proper treatment – mild cases may only need topical therapies, while moderate to severe cases usually require oral medications or aggressive combination treatments.
Can diet and lifestyle factors cause or worsen acne vulgaris?
Yes, certain dietary and lifestyle factors can potentially worsen or trigger flare-ups of acne vulgaris in some individuals, though they are not the sole direct cause.
Diet:
- High glycemic index foods (processed sugars, white bread, etc.) have been linked to increased acne severity, likely due to their effects on hormones and inflammation.
- Dairy products may also exacerbate acne in some people, potentially due to hormones, insulin-spiking effects, or inflammatory components.
- High intake of omega-6 fatty acids vs. low omega-3s may contribute to more inflammation.
- No definitive proven links to acne from things like greasy foods or chocolate.
Lifestyle Factors:
- Stress can indirectly worsen acne by increasing inflammation and altering hormonal levels.
- Lack of sleep is associated with increased acne severity.
- Friction/rubbing from tight clothes, helmets, etc. can aggravate acne lesions.
- Certain medications like lithium, corticosteroids, or anabolic steroids may cause or worsen acne.
- Smoking may exacerbate inflammation and contribute to acne.
However, these dietary and lifestyle influences are not solely responsible for causing acne vulgaris. The underlying factors like hormones, genetics, excess oil production and follicular abnormalities all play a primary role. But modifying diet and lifestyle habits may help some individuals better control their acne alongside medical treatments.
It’s a complex, multifactorial condition – so while diet and lifestyle are not direct root causes, they can potentially alleviate or aggravate acne vulgaris in those already predisposed to developing it.
Is acne vulgaris just a teenage issue or can adults develop it too?
Acne vulgaris is definitely not just a teenage issue – it can persist into adulthood or even first develop later in life for some individuals.
While acne vulgaris is extremely common during adolescence due to the hormonal fluctuations that occur during puberty, many people continue to experience acne breakouts well into their 20s, 30s and beyond.
There are a few key points about adult acne vulgaris:
- For some, the condition simply persists from teenage years and never fully resolves in adulthood, especially for those with more severe, cystic acne.
- In other cases, individuals who did not struggle much with acne as teens can develop acne vulgaris as adults, often triggered by factors like hormonal changes, stress, or certain medications.
- Adult acne is more prevalent among women and can flare with hormone fluctuations from menstrual cycles, birth control, pregnancy, and perimenopause.
- Contributing factors like increased stress, different cosmetic product use, and hormonal imbalances can all set the stage for adult-onset acne vulgaris.
- The lesions tend to favor the lower face, jawline and neck area in adults compared to more widespread patterns in teens.
While it begins in the teenage years for most, acne vulgaris should not be viewed as just a passing condition. It’s estimated that up to 15% of women and 25% of men continue to experience acne into their 30s, and some develop it even later in adulthood. Proper treatment is important at any age.
Can acne vulgaris be prevented or is it inevitable for those genetically predisposed?
While there is no guaranteed way to completely prevent acne vulgaris, especially for those with a strong genetic predisposition, there are some measures that may help reduce the risk and frequency of flare-ups:
Genetic Factors:
- If acne vulgaris runs in the family, an individual is more likely to develop it as well due to inherited factors that influence oil production, hormones, and follicular patterns.
- Those with a close relative with acne are more prone, but severity can still vary based on other influences.
However, even with a genetic tendency, acne vulgaris is not inevitable if preventative steps are taken:
Potential Preventative Measures:
- Follow a consistent, gentle skincare routine to keep pores clear without over-stripping oils.
- Avoid picking/popping lesions to prevent spread of acne-causing bacteria.
- Manage hormonal factors through birth control or medications if appropriate.
- Identify and minimize use of pore-clogging cosmetics, hair products, etc.
- Adopt a healthy lifestyle with good sleep, low stress, nutrition, and exercise.
- Treat mild acne promptly to prevent progression to more severe cases.
Early prevention and sticking to good skincare habits can go a long way, even for the genetically predisposed. However, acne vulgaris may still develop despite best efforts for some individuals who are highly susceptible.
The genetic link makes total prevention difficult. But being proactive about identification and management of triggers can help minimize severity and frequency of outbreaks for many people with an inherited acne tendency. With proper care, flare-ups don’t have to be inevitable.