Folliculitis vs Acne | Acne Skin Guide
Folliculitis and acne are two distinct skin conditions that can sometimes appear similar with red, inflamed bumps. However, they have different causes and require different treatments. Folliculitis is an infection of the hair follicles caused by bacteria, fungi, or inflammation, while acne results from clogged pores, excess oil, and the bacteria Propionibacterium acnes, often triggered by hormones.
Folliculitis bumps are centered on follicles and may have pus, while acne presents as whiteheads, blackheads, or cysts, commonly on the face, back, and chest. Treatments differ, with folliculitis using antibiotics and reducing irritation, while acne requires a multi-pronged approach like retinoids, antibiotics, and procedures. Proper diagnosis by a dermatologist is key, as mismanagement can lead to scarring and other complications for both conditions. Understanding their distinctions allows for effective treatment and prevention through skincare routines and lifestyle modifications.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |

Folliculitis vs Acne: A Comprehensive Guide to Understanding the Differences
Folliculitis and acne are two common skin conditions that can sometimes resemble each other, leading to confusion and improper treatment. While both conditions can cause red, inflamed bumps on the skin, understanding their distinct causes, symptoms, and treatment approaches is crucial for effective management. This comprehensive guide aims to provide an in-depth understanding of the differences between folliculitis and acne, enabling readers to identify and address each condition appropriately.
Causes and Risk Factors
Folliculitis is an infection of the hair follicles caused by various factors, including bacteria, fungi, or inflammatory conditions. Common risk factors for folliculitis include tight clothing, excessive sweating, skin irritation, and exposure to hot tubs or swimming pools. In contrast, acne is primarily caused by a combination of clogged pores, excess oil production, and the presence of bacteria called Propionibacterium acnes. Hormonal changes, certain diets, stress, and genetics play a significant role in the development of acne.
Symptoms and Appearance
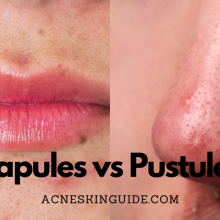
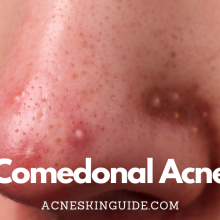
While both folliculitis and acne can result in red, inflamed bumps on the skin, there are distinct differences in their appearance and location. Folliculitis bumps are centered on hair follicles and may appear pus-filled, itchy, or tender to the touch. Acne lesions, on the other hand, typically present as whiteheads, blackheads, or deep, inflamed cysts. Folliculitis can occur anywhere on the body where hair follicles are present, while acne is more commonly found on the face, back, and chest.
Types and Severity
Folliculitis can be classified into several types, including bacterial folliculitis, fungal folliculitis, pityrosporum folliculitis, and pseudofolliculitis barbae (razor bumps). Acne, on the other hand, is categorized based on severity, ranging from mild (a few whiteheads or blackheads) to severe (painful cysts and nodules). Additionally, there are different types of acne, such as cystic acne, hormonal acne, and body acne.
Treatment Approaches
The treatment approaches for folliculitis and acne differ significantly. Folliculitis may be treated with over-the-counter washes and creams, prescription oral antibiotics, or skincare routines aimed at reducing irritation and promoting hygiene. Acne treatment often involves a multi-pronged approach, including topical retinoids and antibiotics, oral medications like isotretinoin, procedural treatments like chemical peels or laser therapy, and natural remedies.
When to Seek Professional Help
It is advisable to consult a dermatologist if home care measures fail to improve the conditions, if there are signs of infection (such as fever or widespread inflammation), or if the bumps are causing significant discomfort or scarring. Seeking professional help ensures accurate diagnosis and appropriate treatment, preventing potential complications and long-term skin damage.
Prevention Strategies
Preventing folliculitis involves avoiding tight clothing, reducing friction and skin irritation, and maintaining good hygiene practices. For acne, prevention strategies include managing hormonal imbalances, following a balanced diet, using appropriate skincare products, and reducing stress levels.
Potential Downsides and Complications
If left untreated or improperly managed, both folliculitis and acne can lead to complications such as permanent scarring, skin discoloration, and negative impacts on self-esteem and mental health. In severe cases, folliculitis can progress to more serious infections, while severe acne can cause deep cystic lesions and increase the risk of scarring.
Special Considerations
Certain populations may require special consideration when dealing with folliculitis and acne. Pregnant women, children/adolescents, and individuals from certain ethnic backgrounds may experience unique presentations or require tailored treatment approaches. It is essential to consult with a dermatologist to ensure appropriate management for these specific groups.
Conclusion
While folliculitis and acne share some similarities in appearance, understanding their distinct causes, symptoms, types, and treatment approaches is crucial for effective management and preventing long-term skin issues. By recognizing the differences between these two conditions, individuals can seek the appropriate care and take proactive steps to maintain healthy, clear skin. Consulting with a dermatologist can provide personalized guidance and ensure the best possible outcomes.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Summary and FAQs
Can stress cause or worsen both folliculitis and acne?
Yes, stress can potentially cause or worsen both folliculitis and acne.
For folliculitis:
Stress can suppress the immune system, making it harder for the body to fight off bacterial or fungal infections that lead to folliculitis. Additionally, increased levels of stress hormones like cortisol can cause inflammation and disrupt the skin’s natural barrier function, making it more susceptible to folliculitis-causing agents.
For acne:
The link between stress and acne is well-established. Stress triggers the release of hormones like cortisol and androgens, which can overstimulate oil glands and lead to excess sebum production, clogged pores, and acne breakouts. Furthermore, stress can also promote inflammation in the skin, exacerbating existing acne lesions.
Stress management techniques, such as regular exercise, meditation, and relaxation practices, can help reduce the impact of stress on both folliculitis and acne by lowering cortisol levels, improving immune function, and minimizing skin inflammation.
It’s important to note that while stress is not the sole cause of these conditions, it can be a significant contributing factor, especially for individuals who are already prone to folliculitis or acne. Addressing stress through lifestyle modifications and seeking professional help if needed can be beneficial in managing both conditions more effectively.
Are there any dietary factors that can influence folliculitis and acne?
Yes, there are several dietary factors that can influence both folliculitis and acne.
For folliculitis:
- High-glycemic diets: Consuming foods with a high glycemic index, such as refined carbohydrates and sugary foods, can increase inflammation in the body and potentially contribute to the development of folliculitis.
- Nutrient deficiencies: Deficiencies in certain nutrients, such as zinc, vitamin A, and vitamin C, may impair the immune system’s ability to fight off infections, including those that cause folliculitis.
For acne:
- Dairy products: Some studies suggest that consuming large amounts of dairy, particularly skim milk, may be linked to an increased risk of acne due to hormonal factors and the presence of specific proteins.
- High-glycemic foods: Similar to folliculitis, a diet high in refined carbohydrates and sugars can promote inflammation and potentially worsen acne.
- Unhealthy fats: Consuming excessive amounts of unhealthy fats, such as trans fats and certain saturated fats, may contribute to increased oil production and clogged pores, which can exacerbate acne.
For both conditions, a diet rich in antioxidants, healthy fats (like omega-3s), and anti-inflammatory foods (such as fruits, vegetables, and whole grains) may help reduce inflammation and support overall skin health.
It’s important to note that individual responses to dietary factors can vary, and a combination of genetic predisposition, hormonal imbalances, and lifestyle factors may also play a role in the development of folliculitis and acne. Consulting a healthcare professional or a registered dietitian can help identify and address any dietary triggers or deficiencies that may be contributing to these conditions.
Can folliculitis and acne coexist or occur simultaneously?
Yes, it is possible for folliculitis and acne to coexist or occur simultaneously in an individual. While folliculitis and acne are distinct skin conditions with different causes, there are scenarios where they can manifest concurrently.
Here are a few reasons why folliculitis and acne may coexist:
- Shared risk factors: Both conditions share some common risk factors, such as hormonal imbalances, excessive sweating, and occlusive clothing or accessories that can trap bacteria and moisture against the skin. These shared risk factors can create an environment conducive to the development of both folliculitis and acne simultaneously.
- Bacterial overgrowth: The bacteria Propionibacterium acnes, which plays a role in the development of acne, can also contribute to certain types of folliculitis, particularly bacterial folliculitis. An overgrowth of this bacteria can potentially lead to the coexistence of both conditions.
- Compromised skin barrier: Individuals with conditions that compromise the skin’s barrier function, such as atopic dermatitis or eczema, may be more susceptible to developing both folliculitis and acne. The impaired barrier allows bacteria and other irritants to penetrate the skin more easily, leading to the simultaneous occurrence of these conditions.
- Secondary infections: In some cases, acne lesions can become infected with bacteria, leading to the development of folliculitis within the existing acne lesions. This can result in a combination of acne and folliculitis occurring together.
It’s important to note that when folliculitis and acne coexist, the treatment approach may need to address both conditions simultaneously. This may involve a combination of therapies targeting bacterial overgrowth, inflammation, and hormonal imbalances, as well as lifestyle modifications to address shared risk factors.
If you are experiencing both folliculitis and acne simultaneously, it is advisable to consult a dermatologist for an accurate diagnosis and appropriate treatment plan tailored to your specific situation.
Are there any genetic or hereditary factors involved in folliculitis and acne?
Yes, there are genetic and hereditary factors that can play a role in the development of both folliculitis and acne.
For folliculitis:
- Genetic predisposition: Some individuals may have an inherited genetic predisposition that makes them more susceptible to developing certain types of folliculitis, such as pseudofolliculitis barbae (razor bumps) or pityrosporum folliculitis.
- Immune system genes: Variations in genes involved in immune system function can influence an individual’s susceptibility to bacterial or fungal infections that lead to folliculitis.
For acne:
- Hereditary factors: Acne has a strong hereditary component. If one or both parents had severe acne, their children are more likely to develop acne as well.
- Genetic variations: Specific genetic variations can influence the production of hormones, sebum, and inflammatory mediators, all of which play a role in the development of acne.
- Ethnic and racial factors: Certain ethnic and racial groups may have a higher prevalence of acne due to genetic factors affecting sebum production and hormonal levels.
It’s important to note that while genetic and hereditary factors can increase the risk of developing folliculitis or acne, they are not the sole determinants. Environmental factors, lifestyle choices, and other underlying health conditions can also contribute to the manifestation of these skin conditions.
Understanding the genetic and hereditary components of folliculitis and acne can help in the following ways:
- Risk assessment: Individuals with a strong family history of these conditions can be more vigilant about preventive measures and early intervention.
- Personalized treatment: Knowing the genetic underpinnings can aid dermatologists in tailoring treatment approaches to the specific genetic variations or predispositions of an individual.
- Ongoing research: Identifying the specific genes and genetic pathways involved can pave the way for the development of more targeted and effective therapies.
While genetic factors play a role, it’s essential to remember that adopting a healthy lifestyle, practicing good skincare habits, and seeking professional medical advice when necessary can help manage and potentially mitigate the impact of folliculitis and acne, regardless of one’s genetic predisposition.
How do folliculitis and acne affect different skin types or ethnicities?
The way folliculitis and acne present and affect individuals can vary depending on different skin types and ethnicities. Here’s an overview of how these conditions may manifest differently across various demographics:
Skin Types:
- Oily skin: Individuals with oily skin types may be more prone to developing acne due to excessive sebum production, which can clog pores and contribute to the formation of comedones (blackheads and whiteheads).
- Dry skin: Those with dry skin may be more susceptible to certain types of folliculitis, such as pityrosporum folliculitis, as the dryness can disrupt the skin’s barrier function and allow for easier entry of microorganisms.
Ethnicities:
- African, African American, and Caribbean ethnicities: These groups are more susceptible to pseudofolliculitis barbae (razor bumps) due to the curved hair follicle shape, which can lead to ingrown hairs and folliculitis after shaving.
- East Asian ethnicities: Acne tends to present with more inflammatory lesions (papules and pustules) in East Asian populations, potentially due to genetic variations in inflammatory pathways.
- Hispanic and Latino ethnicities: Some studies have found a higher prevalence of acne in certain Hispanic and Latino populations, which may be related to genetic factors, hormonal influences, or environmental exposures.
It’s important to note that while these general trends have been observed, individual variability exists within each skin type and ethnic group. Additionally, factors such as age, hormonal changes, and underlying medical conditions can also influence the presentation and severity of folliculitis and acne.
Dermatologists may need to tailor treatment approaches based on the specific skin type and ethnic background of the individual. For example, certain topical treatments or laser therapies may be more effective for different skin types or ethnicities.
Furthermore, cultural practices, such as the use of certain hair products or cosmetics, can also contribute to the development of folliculitis or acne in some communities. Understanding these cultural factors can help in providing more personalized and effective management strategies.
It’s essential for healthcare professionals to be aware of these potential differences and to approach each individual’s case with a culturally sensitive and personalized approach, taking into account their unique skin type, ethnic background, and individual circumstances.