Fungal Acne vs Closed Comedones | Acne Skin Guide
Fungal acne and closed comedones are two distinct skin conditions involving clogged hair follicles, but with different underlying causes and symptoms. Fungal acne is caused by an overgrowth of malassezia yeast and presents as inflamed, itchy bumps, often on the upper body. Closed comedones occur when follicles get clogged with oil and dead skin, appearing as whiteheads or blackheads, mainly on the face.
Treating fungal acne requires anti-yeast products and sometimes oral antifungals, while closed comedones respond to pore-unclogging agents like salicylic acid or retinoids. Prevention involves managing triggers like humidity for fungal acne, and gentle cleansing/exfoliation for closed comedones. Properly diagnosing which condition is present is key, as misidentification can lead to ineffective treatment. If lesions persist despite treatment, seeking professional guidance from a dermatologist is recommended for optimal management of these frustrating but treatable conditions.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |

Distinguishing Between Fungal Acne and Closed Comedones: A Comprehensive Guide
Acne is a common skin condition that affects millions of people worldwide, and it can manifest in various forms, including fungal acne and closed comedones. While both conditions involve clogged hair follicles, they have distinct causes, symptoms, and treatment approaches. Understanding the differences between fungal acne and closed comedones is crucial for effective management and prevention.
Causes and Triggers
Fungal acne, also known as pityrosporum folliculitis or malassezia folliculitis, is caused by an overgrowth of the naturally occurring malassezia yeast on the skin. This condition is often triggered by factors that create a warm, humid environment conducive to yeast growth, such as excessive sweating, tight clothing, and high humidity levels. Additionally, underlying conditions like diabetes or a weakened immune system can increase the risk of developing fungal acne.
On the other hand, closed comedones, which include whiteheads and blackheads, occur when hair follicles become clogged with a buildup of sebum (oil), dead skin cells, and other debris. Hormonal changes, particularly during puberty or menstrual cycles, can stimulate increased oil production and contribute to the formation of closed comedones. Furthermore, the use of heavy, pore-clogging moisturizers and makeup products can exacerbate the problem.
Symptoms and Appearance
Fungal acne typically presents as clusters of inflamed, itchy, red bumps or pustules, often concentrated on the upper body, back, and chest areas. These lesions may appear similar to traditional acne but are typically accompanied by intense itching, which is a hallmark symptom of fungal acne.
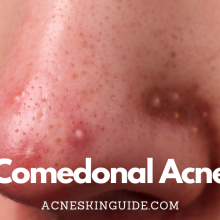
In contrast, closed comedones appear as small, skin-colored or blackish bumps on the skin’s surface. Whiteheads are closed, flesh-toned bumps, while blackheads have a central darker portion due to the exposure of the clogged material to air. Closed comedones are generally non-inflamed and do not cause itching or discomfort.
One of the key distinguishing features between fungal acne and closed comedones is their distribution pattern on the body. While fungal acne tends to concentrate on the upper body, back, and chest, closed comedones are more commonly found on the face, particularly in areas with a higher concentration of oil glands, such as the forehead, nose, and chin.
Treatments and Management
Effective treatment for fungal acne involves addressing the underlying yeast overgrowth. Over-the-counter products containing selenium sulfide or zinc pyrithione can help control the malassezia yeast population. For more severe cases, prescription oral antifungal medications may be necessary to achieve long-term relief.
In contrast, closed comedones are typically treated with salicylic acid-based products or retinoids like Differin, which help unclog pores and promote exfoliation. Over-the-counter salicylic acid cleansers and masks can be effective for mild cases, while prescription-strength retinoids are often recommended for more stubborn or widespread closed comedones.
Prevention strategies for fungal acne include using anti-yeast skincare products and making lifestyle changes to reduce sweat and humidity exposure, such as wearing breathable fabrics and using air conditioning in warm, humid environments. For closed comedones, regular gentle cleansing and exfoliation can help remove pore-clogging agents and prevent future buildup.
Potential Downsides and Considerations
While both fungal acne and closed comedones can be frustrating and impact self-confidence, it’s essential to avoid picking or popping any lesions. Doing so can lead to further inflammation, scarring, and the potential spread of the underlying microbes or debris.
It’s also crucial to rule out other types of acne, such as bacterial or hormonal acne, as the treatment approaches differ. Misdiagnosing the condition can lead to ineffective treatment and prolonged frustration.
Additionally, some individuals may experience side effects or skin irritation from certain treatments, particularly with prescription-strength products. It’s always advisable to follow the instructions carefully and consult a dermatologist if any adverse reactions occur.
Conclusion
Fungal acne and closed comedones are distinct skin conditions that require different treatment approaches. While both involve clogged hair follicles, their underlying causes, symptoms, and effective treatments vary significantly. Proper diagnosis and understanding of these differences are essential for successful management and prevention.
If you’re unsure about the nature of your skin lesions or if they persist despite treatment, seeking guidance from a dermatologist is highly recommended. A professional evaluation can help identify the root cause and develop a tailored treatment plan for your specific condition, ensuring optimal results and minimizing potential downsides or complications.
Remember, consistency and patience are key when managing any skin condition. With the right approach and dedication, both fungal acne and closed comedones can be effectively controlled, leading to clearer, healthier skin.
#1 Recommended Acne Treatment | #2 Recommended Acne Treatment |
 |  |
Summary and FAQs
Can fungal acne and closed comedones occur together?
Yes, it is possible for fungal acne (pityrosporum folliculitis) and closed comedones (whiteheads and blackheads) to occur together on the same person’s skin. These two conditions have different underlying causes, but they can coexist and affect the same areas of the body.
Fungal acne is caused by an overgrowth of the yeast Malassezia, which naturally lives on human skin. When this yeast proliferates excessively, it can lead to inflamed, itchy bumps or pustules, often concentrated on the upper body, back, and chest.
On the other hand, closed comedones are clogged hair follicles filled with a combination of oil, dead skin cells, and other debris. These can appear as whiteheads (closed bumps) or blackheads (open bumps with a dark central portion).
It’s not uncommon for individuals, particularly those with acne-prone skin, to experience both fungal acne lesions and closed comedones simultaneously or in close proximity. The presence of one condition does not necessarily preclude the other, as they can stem from different underlying factors.
However, it’s important to note that having both conditions at the same time can make proper diagnosis and treatment more challenging, as the treatment approaches may differ slightly. In such cases, consulting a dermatologist can help determine the most effective combination of therapies to address both the fungal overgrowth and the clogged pores contributing to the closed comedones.
How long does it typically take to see improvement with treatment?
The timeline for seeing improvement when treating fungal acne or closed comedones can vary depending on the specific condition, the severity of the breakout, and the type of treatment being used. However, here are some general guidelines:
For Fungal Acne (Pityrosporum Folliculitis):
- With over-the-counter antifungal treatments (e.g., selenium sulfide, zinc pyrithione): You may start to see some improvement within 2-4 weeks of consistent use.
- With prescription oral antifungal medications: Improvement is often seen within 4-6 weeks, though it can take up to 12 weeks for complete clearance in severe cases.
For Closed Comedones (Whiteheads and Blackheads):
- With over-the-counter salicylic acid products: You may notice a reduction in comedones within 4-8 weeks of regular use.
- With prescription retinoids (e.g., tretinoin, adapalene): Initial improvement can be seen in 4-8 weeks, but it may take 3-6 months to achieve maximum comedone clearance.
It’s important to note that patience and consistency are key when treating any acne condition. Stick with the recommended treatment regimen for at least 8-12 weeks before evaluating its effectiveness, as it can take time for the products to fully work on deeply clogged pores or stubborn fungal overgrowth.
Additionally, factors like hormonal fluctuations, stress levels, and adherence to a proper skincare routine can also influence the rate of improvement. If you don’t see satisfactory results within a reasonable timeframe, it’s best to consult a dermatologist for further evaluation and potential adjustments to your treatment plan.
Are there any specific dietary or lifestyle factors that can influence the development of fungal acne or closed comedones?
Yes, there are several dietary and lifestyle factors that can potentially influence the development or exacerbation of fungal acne (pityrosporum folliculitis) and closed comedones:
Fungal Acne:
- High sugar/refined carb intake: A diet high in sugary foods and refined carbohydrates can promote yeast overgrowth, including the Malassezia yeast responsible for fungal acne.
- Excessive sweating: Activities or environments that cause heavy sweating can create a moist, warm environment conducive to yeast proliferation.
- Humidity: Living or spending extended periods in humid climates can increase the risk of fungal acne flare-ups.
Closed Comedones:
- High-glycemic diet: Foods that rapidly spike blood sugar levels can stimulate excess oil production, potentially leading to clogged pores and comedones.
- Dairy products: For some individuals, consuming dairy may contribute to increased oil production and comedone formation due to hormonal effects.
- High-fat, greasy foods: A diet rich in fried or greasy foods can worsen comedonal acne by increasing oil secretion and clogging pores.
- Stress: High stress levels can disrupt hormone balance, leading to excess oil production and potentially more comedones.
Lifestyle factors for both conditions:
- Not removing makeup properly: Leaving makeup on overnight can clog pores and exacerbate both fungal acne and closed comedones.
- Friction from tight clothing/hats: Clothing or accessories that rub against the skin can worsen both conditions by spreading bacteria, yeast, or debris into hair follicles.
- Poor hygiene: Infrequent cleansing or showering, especially after sweating, can allow yeast, oil, and dead skin cells to accumulate, worsening breakouts.
While these factors don’t directly cause fungal acne or closed comedones, they can create an environment that promotes their development or makes existing conditions worse. Maintaining a balanced diet, managing stress, and practicing good hygiene habits can help mitigate the risk of flare-ups for both conditions.
Can fungal acne or closed comedones lead to permanent scarring?
Yes, both fungal acne and closed comedones have the potential to lead to permanent scarring if they are not treated properly or are allowed to persist for an extended period of time.
Fungal Acne (Pityrosporum Folliculitis):
- The inflamed, itchy bumps and pustules associated with fungal acne can develop into deeper lesions if scratched, picked, or left untreated.
- These deeper lesions can rupture and damage the surrounding skin, leading to the formation of pitted or raised scars.
- Prompt treatment with antifungal medications and avoiding picking/squeezing the bumps can help prevent scarring from fungal acne.
Closed Comedones (Whiteheads and Blackheads):
- While closed comedones themselves are non-inflamed lesions, they can sometimes become inflamed if bacteria or other irritants get inside the clogged pore.
- Inflamed comedones (papules or pustules) have a higher risk of leading to permanent scarring, especially if picked or squeezed forcefully.
- Picking and aggressive extraction of comedones can also cause trauma and scarring to the surrounding skin.
- Consistent treatment with comedolytic agents (like salicylic acid or retinoids) and avoiding picking can minimize the risk of scarring from closed comedones.
It’s important to note that some individuals are more prone to scarring than others due to genetic factors or skin type. Those with darker skin tones may be at a higher risk of developing hyperpigmented (darker) or hypopigmented (lighter) scars from any type of acne lesion.
Seeking professional treatment from a dermatologist, especially for severe or persistent cases of fungal acne or comedonal acne, can help prevent scarring and manage the conditions effectively. Early intervention and avoiding manipulation of the lesions are key to reducing the risk of permanent scarring.
Are there any over-the-counter products that can effectively treat both fungal acne and closed comedones?
There are a few over-the-counter (OTC) products that can potentially help treat both fungal acne (pityrosporum folliculitis) and closed comedones (whiteheads and blackheads), but their effectiveness may vary depending on the severity of the conditions.
- Salicylic Acid products:
Salicylic acid is a beta-hydroxy acid that can help treat both fungal acne and closed comedones. It has keratolytic and comedolytic properties, which means it can help shed dead skin cells, unclog pores, and dry out excess oil.
For fungal acne, salicylic acid can help reduce the yeast overgrowth and clear up the inflamed bumps and pustules. For closed comedones, it can help dissolve the built-up oil and debris within the clogged pores.
OTC salicylic acid products come in various forms, such as cleansers, toners, spot treatments, and masks. Look for concentrations ranging from 0.5% to 2% for daily use.
- Benzoyl Peroxide products:
Benzoyl peroxide is an antibacterial and anti-inflammatory agent commonly used in acne treatments. While it is primarily effective against bacterial acne, it can also help reduce the inflammation and pustules associated with fungal acne.
Additionally, benzoyl peroxide has mild keratolytic properties, which means it can help shed dead skin cells and unclog pores, potentially improving closed comedones.
OTC benzoyl peroxide products typically range from 2.5% to 10% concentrations and come in various forms, such as gels, creams, and cleansers.
- Sulfur products:
Sulfur has antimicrobial and anti-inflammatory properties, making it potentially beneficial for both fungal acne and closed comedones. It can help dry out excess oil and clear out clogged pores.
OTC sulfur products, such as soaps, lotions, and masks, may contain varying concentrations of sulfur, typically ranging from 2% to 10%.
While these OTC products can be helpful for mild to moderate cases of fungal acne and closed comedones, it’s important to note that they may not be as effective as prescription-strength treatments for severe or persistent conditions. Additionally, some individuals may experience dryness, irritation, or other side effects from these products.
If you don’t see significant improvement after several weeks of consistent use, or if your condition worsens, it’s recommended to consult a dermatologist for a proper evaluation and prescription-strength treatments tailored to your specific needs.